When the effects of a drug are altered by the presence of another drug or drugs as a result of coadministration, it is termed a drug-drug interaction (DDI). In developed countries, DDIs continue to be a significant public health concern, contributing to adverse drug reactions, hospital admissions, and even deaths. 1,2
Despite advances in our mechanistic understanding of how drugs interact, many DDIs remain undetected or underrecognized in clinical practice. This persistent challenge has motivated researchers to explore artificial intelligence (AI) and machine learning approaches to enhance our ability to detect and predict DDIs.
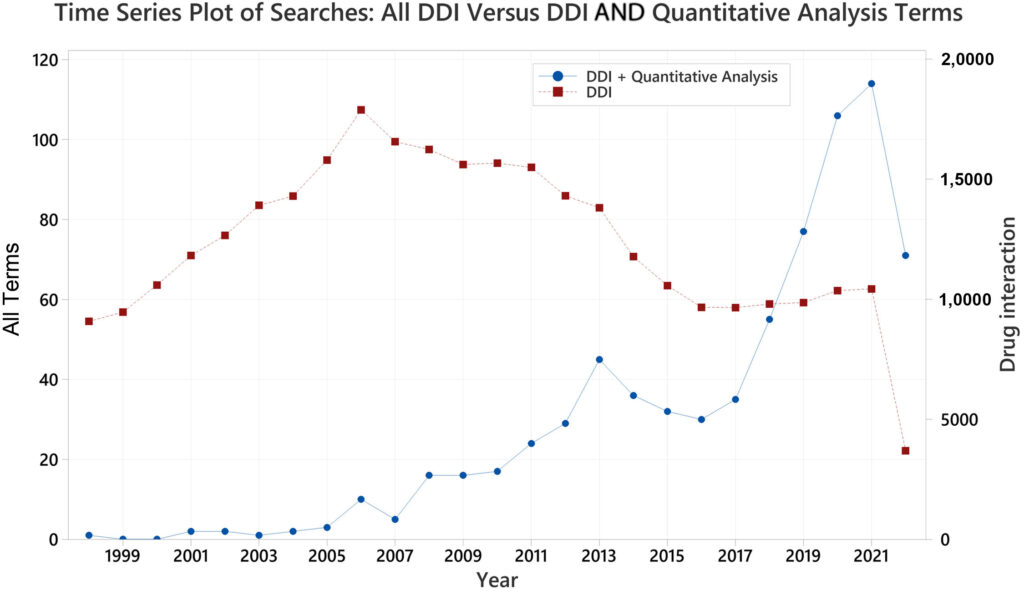
Ever since I stumbled upon this article by Manfred Hauben, I have followed the rapid growth of AI applications in the DDI space with great interest. A literature search reveals an exponential increase in publications on AI for DDI detection and prediction over the past decade (Figure 1 in Hauben’s article, attached below). This surge of research activity reflects both the promise and the complexity of leveraging AI to tackle this longstanding problem.
In this article, I will provide an overview of the key AI approaches explored for DDI detection and prediction, discuss their potential benefits and limitations, and offer some thoughts on the path forward. My aim is to cut through some of the hype and provide a balanced perspective on where we stand with AI for DDIs.
The Persistent Challenge of Undetected DDIs
Before we talk about the various AI approaches to this problem, it’s important to reflect on why DDIs continue to evade manual detection despite our growing mechanistic knowledge. There are several key factors at play:
- Combinatorial complexity: With the ever-increasing number of approved drugs and the prevalence of polypharmacy, the number of potential DDI combinations has exploded. This makes it challenging to test all possibilities.
- Biological complexity: DDIs can occur through multiple, interconnected biological pathways. Some interactions may only manifest in the presence of certain diseases or genetic variants.
- Limited pre-approval testing: Clinical trials cannot feasibly test all potential drug combinations across diverse patient populations.
- Underrepresented populations: Children, elderly patients, and those with rare genetic variants are often excluded from DDI studies.
- Unknown mechanisms: Despite advances, the mechanisms of some DDIs remain poorly understood, making detection difficult.
These factors create a perfect storm that allows some DDIs to slip through the cracks of traditional detection methods. AI approaches offer the tantalizing possibility of sifting through vast amounts of data to uncover hidden interaction patterns that humans may miss.
Key AI Approaches for DDI Detection and Prediction
The AI landscape for DDIs can be broadly divided into two categories: “prediction” and “detection” approaches.
Prediction approaches tend to focus on leveraging chemical, biological, and pharmacological knowledge bases to forecast potential DDIs for new or existing drugs. These methods often aim to support drug development by flagging potential interactions early.
Detection approaches, on the other hand, typically mine real-world data sources like spontaneous reporting systems, electronic health records, and claims databases to identify novel adverse DDI signals for drugs already on the market.
Finding the article useful?
This is an Open Access Newsletter, which means the author has kept this free for academic interests. For getting free articles on AI in Medicine like these in your inbox, join the newsletter.
While there is some overlapbetween prediction and detection approaches, I’ll discuss key methods in each category:
Prediction Approaches:
Similarity Analysis:
This is one of the most common prediction approaches. The core idea is that if drug A is known to interact with drug B, and drug C is very similar to drug A across multiple chemical and biological properties, then drug C is likely to also interact with drug B.
Researchers use various similarity metrics to compare drugs, including 2D and 3D chemical structures, interaction profiles, protein targets, biological pathways, side effects, and more.3 These similarities are often combined into integrated similarity scores.
Machine learning classifiers like support vector machines or neural networks can then be trained on these similarity features to predict whether a given drug pair is likely to interact.
Network-based Methods:
These approaches leverage the complex web of known drug-protein, protein-protein, and drug-drug interactions to make predictions. Graph neural networks and other techniques can learn patterns in these biological networks to forecast potential DDIs.4
Natural Language Processing: Some researchers are using NLP to mine the biomedical literature and extract DDI information that can be used to train predictive models.
Detection Approaches:
- Disproportionality Analysis: This statistical approach looks for drug-event pairs that occur more frequently than expected in spontaneous reporting databases. It can be extended to drug-drug-event triplets to detect potential DDI signals.5
- Association Rule Mining: This technique searches for frequent co-occurrence patterns in data to generate “if-then” rules about potential DDIs.6
- Logistic Regression: Researchers have used logistic regression models on spontaneous reports and other data sources to identify DDI signals, sometimes incorporating regularization techniques to handle large numbers of predictors.7
- Neural Networks: Various neural network architectures are being explored to detect DDI signals in electronic health records and other clinical data sources.
Promises and Problems of AI for DDIs
The surge of AI research in this space has produced some impressive results in controlled studies. Many of the prediction approaches report high accuracy, with AUC values over 0.9 in some cases.8 Detection methods have also shown promise in identifying known DDIs and generating novel hypotheses.
However, it’s crucial to approach these results with a healthy dose of skepticism and understand their limitations. Here are some key considerations:
- Data quality and biases: AI models are only as good as the data they are trained on. Many studies rely on DDI databases or spontaneous reports that may contain inaccuracies or biases. We need to be cautious about perpetuating these biases in AI predictions.
- Lack of mechanistic insight: While AI can identify statistical associations, it often cannot explain the underlying biological mechanisms. This “black box” nature can make it challenging for clinicians and regulators to trust and act on AI-generated DDI signals.
- Difficulty in prospective validation: Most studies evaluate AI models retrospectively on known DDIs. Prospective validation in real-world clinical settings is much more challenging and rarely done.
- Overconfidence and automation bias: There’s a risk that impressive-sounding AI results may lead to overconfidence in the technology, potentially overshadowing clinical judgment.
- Limited real-world impact: Despite the proliferation of AI studies, their actual impact on reducing DDI-related adverse events in clinical practice remains to be demonstrated.
Integrating AI into Holistic Pharmacovigilance
While the limitations are significant, I believe AI has an important role to play in enhancing DDI detection and prediction. The key is to view AI as one tool in a broader, holistic approach to pharmacovigilance.
Here are some thoughts on how we can responsibly integrate AI into DDI surveillance:
- Combine multiple data sources and methods: Instead of relying on a single AI approach, we should leverage diverse data streams and analytical techniques. This can help overcome the limitations of individual methods and data sources.
- Incorporate domain knowledge: We should strive to develop AI models that can integrate mechanistic knowledge about drug interactions rather than purely relying on statistical associations.
- Focus on interpretability: Developing more interpretable AI models that can provide insights into potential DDI mechanisms will be crucial for clinical adoption.
- Rigorous validation: We must emphasize prospective, real-world validation of AI-generated DDI signals before they influence clinical practice.
- Human-AI collaboration: Rather than viewing AI as a replacement for human expertise, we should focus on how AI can augment and support clinical decision-making around DDIs.
- Ethical considerations: As we deploy AI systems, we must be vigilant about potential biases and unintended consequences, especially for vulnerable populations.
The application of AI to DDI detection and prediction is a rapidly evolving field with immense potential. While the current research shows promising results, we must temper our enthusiasm with a realistic understanding of the challenges and limitations.
As we move forward, the goal should be to thoughtfully integrate AI approaches into comprehensive pharmacovigilance systems that combine the strengths of machine learning with human clinical expertise. By doing so, we can work towards the ultimate goal of reducing the public health burden of drug-drug interactions and improving patient safety.
References:
- Magro L, Moretti U, Leone R. Epidemiology and characteristics of adverse drug reactions caused by drug-drug interactions. Expert Opin Drug Saf. 2021;11:83-94. ↩︎
- Dechanont S, Maphanta S, Butthum B. Hospital admissions/visits associated with drug-drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23:489-497. ↩︎
- Vilar S, Uriarte E, Santana L, et al. Similarity-based modeling in large-scale prediction of drug-drug interactions. Nat Protoc. 2014;9:2147-2163. ↩︎
- Zitnik M, Agrawal M, Leskovec J. Modeling polypharmacy side effects with graph convolutional networks. Bioinformatics. 2018;34:i457-i466. ↩︎
- Noguchi Y, Tachi T, Teramachi H. Review of statistical methodologies for detecting drug-drug interactions using spontaneous reporting systems. Front Pharmacol. 2019;10:1319. ↩︎
- Noguchi Y, Ueno A, Otsubo M, et al. A new search method using association rule mining for drug-drug interaction based on spontaneous report system. Front Pharmacol. 2018;9:197. ↩︎
- van Puijenbroek EP, Egberts AC, Heerdink ER, Leufkens HG. Detecting drug-drug interactions using a database for spontaneous adverse drug reactions: an example with diuretics and non-steroidal anti-inflammatory drugs. Eur J Clin Pharmacol. 2000;56:733-738. ↩︎
- Vo TH, Nguyen NTK, Kha QH, Le NQK. On the road to explainable AI in drug-drug interactions prediction: a systematic review. Comput Struct Biotechnol J. 2022;20:2112-2123. ↩︎
